Unraveling the Psychological Consequences of Obesity on Adult Quality of Life
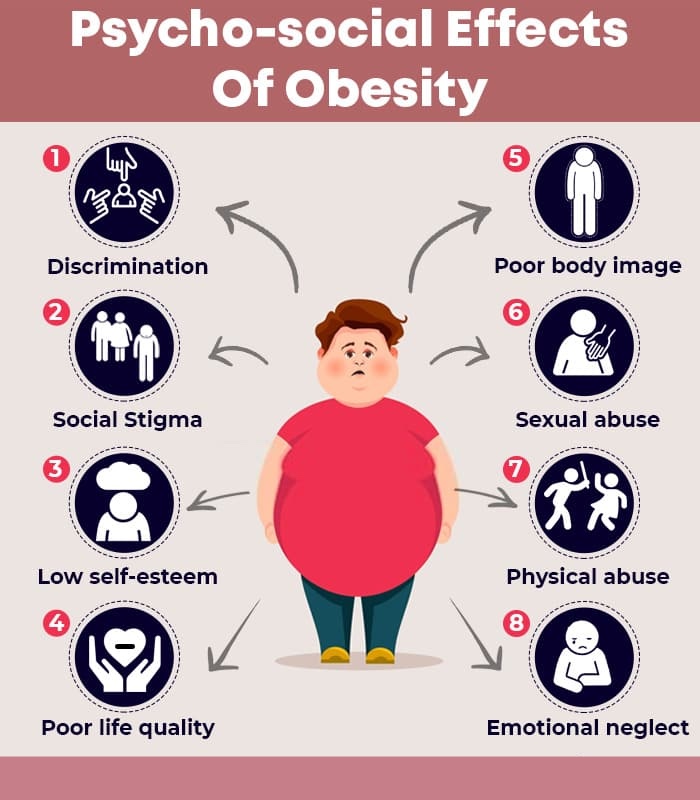
Obesity is a multifaceted health concern affecting millions of adults worldwide. Beyond the physical implications, the psychological consequences associated with excess weight play a pivotal role in shaping the quality of life for individuals dealing with obesity. Recent estimates indicate that a significant percentage, ranging from 20 to 60 percent, of adults with obesity grapple with psychological challenges. These consequences, including depression, stress, low self-esteem, and impaired body image, intricately weave into the fabric of an individual’s overall well-being.
The Concept of Quality of Life:
Quality of life is a nuanced construct that encompasses an individual’s evaluation of their well-being in the spheres of physical and mental health, social relationships, and economic factors. Recognizing the interplay between psychological factors and obesity is gaining prominence in healthcare, as comprehensive patient care increasingly involves understanding the bio-psychosocial impact of weight on well-being.
The Complex Relationship Between Obesity and Depression:
The link between obesity and depression is intricate and bidirectional. Research reveals that excess weight can contribute to the onset of depression, while conversely, depression and the use of antidepressants can lead to unwanted weight gain. Gendered differences are also evident, with women experiencing depression more frequently in the context of obesity. A meta-analysis highlights the complexity of this relationship, finding positive, negative, or no correlation between depression and obesity. A systematic review further suggests that adults with obesity are more prone to depression compared to their healthy-weight counterparts.
Insights from Longitudinal Studies:
Longitudinal studies provide valuable insights into the enduring impact of weight on mental health. In a study following 58,000 participants for 28 years, those who were overweight at the study’s commencement faced a 55 percent increased risk of depression. Simultaneously, participants who were depressed at the study’s outset had a 58 percent likelihood of experiencing unwanted weight gain. These findings underscore the intricate interplay between mental health and obesity over the long term.
Low Self-Esteem and Its Connection to BMI:
Low self-esteem emerges as another psychological consequence tightly entwined with obesity. Research indicates a correlation between low self-esteem and a higher body mass index (BMI), underscoring the importance of addressing the emotional dimensions of obesity. This relationship adds another layer to the complex interplay of psychological factors affecting individuals with excess weight.
Mitigating Psychological Consequences: A Comprehensive Approach:
To address the psychological consequences associated with excess weight, diet and lifestyle coaches must adopt a holistic approach. Recognizing the intricate links between depression, self-esteem, and overall quality of life, clinicians should prioritize the psychosocial health of patients alongside physiological and metabolic considerations.
Social Isolation and Loneliness: A Consequence of Low Self-Esteem:
For adults with obesity, the negative impact on self-esteem may lead to withdrawal from social interactions and activities, fostering isolation and loneliness. These emotional repercussions can exacerbate depression and other psychological challenges. Diet and lifestyle coaches should engage with patients to understand how their quality of life affects their psychological well-being, fostering a patient-centered approach that considers the whole individual.
The Role of Mental Health Professionals:
Referrals to mental health professionals might be a crucial component of the treatment protocol for adults with obesity. Collaborative efforts with mental health practitioners can address the psychological dimensions of obesity, promoting overall well-being. This integrated approach ensures that patients receive comprehensive care, acknowledging the complex interplay between mental and physical health.
Nutritional Interventions for Improved Well-Being:
In addition to mental health support, lifestyle coaches can work with patients to develop sustainable, healthy eating plans. These plans, complemented by pre-packaged, nutritionally formulated meal replacements, offer convenience while meeting daily recommendations for essential vitamins and minerals. Low Calorie Diets (LCD) or Very Low Calorie Diets (VLCD) can be considered as part of an overall strategy to promote a healthy lifestyle.
Understanding and addressing the psychological consequences of obesity is paramount for enhancing the quality of life for affected individuals. As we delve into the complexities of this relationship, a patient-centered and comprehensive approach is essential. By considering the bio-psychosocial impact of weight on well-being, clinicians can empower individuals to navigate the challenges of obesity, fostering a holistic journey towards improved health and a better quality of life.