The Importance of a Solid Meal Plan While Using Weight Loss Shots
In the quest for effective weight loss, many individuals turn to GLP-1 medications to help suppress their appetite. While these medications can be a valuable tool in achieving weight loss goals, it’s crucial to emphasize the need for a solid meal plan. Simply relying on appetite suppression without proper nutrition can lead to serious health concerns, such as nutritional deficiencies, muscle wasting, and a slowed metabolism. In this blog post, we will explore why a balanced meal plan is essential when utilizing GLP-1 medications and how incorporating ideal protein meal replacements can support overall health during the weight loss journey.
The Pitfalls of Suppressing Appetite Without a Meal Plan:
- Nutritional Deficiencies:
Appetite suppression can inadvertently lead to a reduction in food intake, putting individuals at risk of nutritional deficiencies. Our bodies require a diverse range of nutrients, including vitamins, minerals, and essential amino acids, to function optimally. Ignoring these nutritional needs can result in fatigue, weakness, and other health complications.
- Muscle Wasting and Metabolic Slowdown:
Lack of protein intake is a common consequence of reduced appetite. Protein is essential for maintaining muscle mass, and inadequate consumption can lead to muscle wasting. As muscles play a crucial role in boosting metabolism, their deterioration can result in a slowed metabolic rate, making it easier to regain weight once the medication is discontinued.
- Organ Health Concerns:
Many critical organs in our body are either muscles or composed of protein. Neglecting proper nutrition may compromise the health of these organs, potentially leading to long-term health issues. Maintaining a balanced meal plan ensures that these vital organs receive the nutrients they need for optimal functioning.
The Role of Ideal Protein Meal Replacements:
- Convenience and Accessibility:
Ideal protein meal replacements offer a convenient and accessible solution for individuals using GLP-1 medications. These replacements are compact and require minimal effort to consume, making them ideal for those with a suppressed appetite. They provide a concentrated source of essential nutrients without the need for large meals.
- Essential Amino Acids Support:
Ideal protein meal replacements are carefully formulated to contain all the essential amino acids our bodies need. Amino acids are the building blocks of protein, crucial for maintaining muscle mass and supporting various physiological functions. By incorporating these meal replacements, individuals can ensure that their bodies receive the necessary protein without relying solely on traditional meals.
- Long-Term Health and Weight Maintenance:
Weight loss is not just about shedding pounds; it’s about fostering long-term health and maintaining a healthy weight. Utilizing GLP-1 weight loss shot medications alongside a well-rounded meal plan, including ideal protein meal replacements, helps address immediate weight loss goals while laying the foundation for sustained health and well-being.
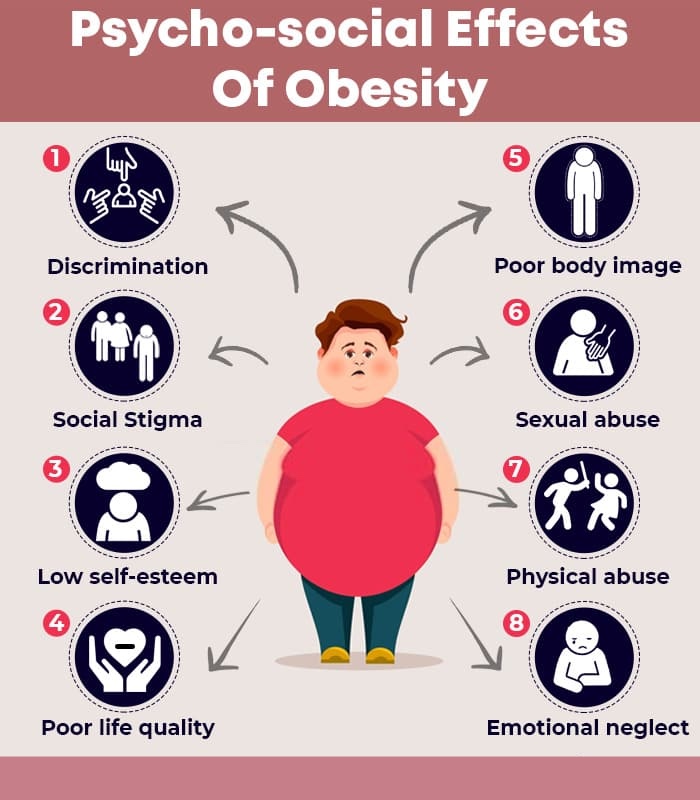
- Addressing the Relationship with Food:
It’s essential to recognize that using medications alone does not address the root cause of weight-related issues—the relationship with food. Incorporating a solid meal plan encourages mindful eating habits and fosters a positive approach to nutrition. Developing a healthier relationship with food is crucial for sustained weight management and overall well-being.
While GLP-1 medications (shots for appetite suppression) can be effective in aiding weight loss in the short term, it’s imperative to approach this strategy with a comprehensive meal plan. Ignoring nutritional needs, especially protein requirements, can have detrimental effects on muscle mass, metabolism, and organ health. Ideal protein meal replacements offer a practical solution to ensure essential nutrient intake without relying solely on traditional meals. By prioritizing a balanced meal plan, individuals can achieve sustainable weight loss while promoting long-term health and well-being. Additionally, addressing the psychological aspects of eating is crucial for establishing a healthy relationship with food that extends beyond the use of medications.